This post is long so I’ll keep the intro short.
Here I take a look at the root causes of burnout and provide physician-specific context and examples along the way.
Please note that I’ve previously written on charting being the leading cause of burnout based on surveyed physician data. As you’ll see in this post, there are underlying reasons for why charting is leading cause.
I'm Burnin', I'm Burnin', I'm Burnin' (Out) For You
“You” being Dr. Christina Maslach. If you’re talking about anything burnout-related, then, whether you realize it or not, you’re referencing Dr. Maslach’s pioneering work.
She has dedicated her career to research on the definition, predictors, and measurement of workplace burnout. You’ve probably heard of her eponymous Maslach Burnout Inventory (MBI), which is the most widely used instrument for measuring burnout.
It is through her endeavors and the groundwork she laid that that the World Health Organization (WHO*) listed burnout as an occupational phenomenon with health consequences, thus allowing burnout to make it into the ICD-10 and -11.
*I’m one of the rare few who doesn’t read out the letters and instead reads it as the word/pronounces it “hoo”
Says WHO
Backing up just a little bit:
Burnout is defined in the ICD-11 as “a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed.”
The last part in that definition always gives me pause. I know it’s not implying any fault of the individual, but just that chronic stress does not always lead to burnout.
However, the “successfully managed” phrasing makes it sound like a failure, which I don’t like. Too bad the WHO didn’t consult me, and probably never will since I keep calling them the “hoo.”
Burnout is experienced in three broad dimensions:
- Emotional exhaustion
- Depersonalization/cynicism
- Reduced personal efficacy
From Burnout to Engagement
Maslach and colleague Michael Leiter have previously elaborated that burnout is on a continuum at one end, with engagement at the opposite end. This continuum utilizes the same above three dimensions with alternate labels: energy, involvement, and effectiveness.
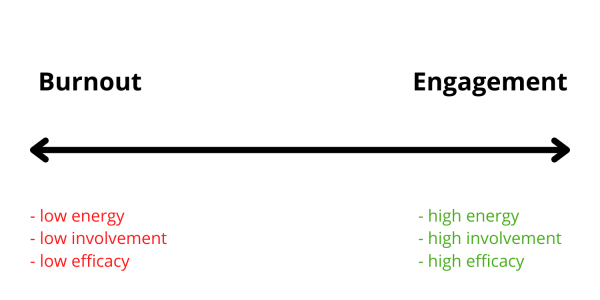
Burnout is when all three dimensions are deficient: low energy, low involvement, and low efficacy.
Engagement, on the other hand, is when all three are in excess: high energy, high involvement, and high efficacy.
The utility of the continuum is that it demonstrates that burnout should not be simply reduced to a binary outcome—present or absent—much as we refer to it as such, but instead should be viewed as a more complex and nuanced process.
I think it is intuitive that “burnout may develop differently under different environmental conditions” and thus be “present to varying degrees.” (These quotes are from article linked just below).
Mishmash? Mismatch?
Maslach and Leiter also investigated and proposed six areas of work life in which burnout can occur based on organizational conditions. They are described here in a short article on which this post is based.
These are not specific to healthcare, but I think as you read through them, they’ll resonate to varying degrees with your own experiences.
The six work life areas are:
- Workload
- Control
- Reward
- Community
- Fairness
- Values
According to Maslach and Leiter in the above article, “Burnout arises from chronic mismatches between people and their worksetting [sic] in terms of some or all of these six areas.”
The operative word above is “mismatch.” The issue at play with each area above is not the employers’ and individuals’ needs or requirements, but instead the interplay between them—the relationship.
The wider the disparity in the relationship—between an employer’s expectations & rules and an individual’s goals & wishes—the larger the mismatch and the greater the chance that burnout may develop in this area.
Sort of like the myriad mismatches in our glove sizes—I mean, judicial system.
For the purposes of this post, I am minimizing these complex relationships in each work area into “causes” of burnout.
The remainder of this post will explore each of these “causes” in more depth as presented in the article referenced above.
1. Workload
There is a direct relationship between increasing workload and worsening burnout. It is especially tied to the dimension of emotional exhaustion.
Those who conduct demanding work need time to recover and recuperate. If this time is not provided and/or the work exceeds their limits consistently, then exhaustion is almost guaranteed.
I can’t help but chuckle at this because it sounds like the tagline for residency training: “You show up. We grind you down. Rinse and repeat.”
During my interview with Dr. Jimmy Turner on The Physician Philosopher Podcast, I quipped that residency was putting Care Bears through marine training and intending for them to come out intact Care Bears on the other side. It’s folly.
Maslach and Leiter specifically call out the human service sector (of which healthcare is a part) as being the most egregious with workload demands. This is in large part due to the emotionality involved in the helping relationships required in medicine, for example.
Furthermore, lines between work and life outside of work are blurred with such emotional work making it harder to decompress and recover.
“Although service providers often entered their professions seeking emotionally involving work, their institutional context was not structured in a way that permitted an enduring participation in demanding work.”
And yet we endure. And thus we burnout.
Workload mismatch impacts burnout the most compared to the other work life areas. If the other five were the Planeteers, then workload would certainly be Captain Planet.
Okay, that was a terrible analogy full of holes, but it let me work in a Captain Planet reference, so it’s a win in my books!
2. Control
Control here is defined as autonomy and the lack of ambiguity or conflict in fulfilling one’s role.
Sound like something you experience? Hah. Mismatches abound!
Contradictory demands on our time cause much dissatisfaction. At any given moment in my primary care clinic, I’m juggling seeing patients, responding to calls and messages, reviewing test results, filling out paperwork, and on and on.
You all have these same pressures on your time that take you away from performing your highest functions consistently, be it diagnosing, treating, or procedurizing (my made up word).
Any work that does not involve these things prevents us from performing at the top of our capabilities and licensure, which is a disservice to us and society at large, especially in light of physician shortages. Worse still, this work spills over into our time that is supposed to be away from work, further compounding workload issues.
Even surgeons in the OR are unable to commit themselves fully to a surgical case because they get interrupted, for example, by their pager going off.
See what happens when you interrupt a surgeon?
I discuss this in my online course and coaching program, Charting Conquered, in a module that covers deep work, interruptions, and decision fatigue.
I want to point out something interesting under this work life area: private practice docs tend to work harder to keep their doors open, but overall experience less burnout, which seems at odd with the workload area.
This phenomenon is attributable to the autonomy inherent in their practice, even if only autonomy over their immediate micro-environment (i.e., their workflows and team structure), which also helps them better align their work with their values. This seems to be protective against the healthcare landscape at large like dealing with insurance company woes.
3. Reward
This one is also straightforward: insufficient reward, be it financial, recognition, or social, for work completed can lead to burnout.
How many of you feel underpaid? How many of you feel like you’re taken for granted—a cog in the machine? How many of you feel isolated from your colleagues because you have no time to even visit with them due to the breakneck speed at which you’re being told you have to work? This last one plays into the community work life area below.
Recognition plays into the third dimension of burnout; we feel a sense of personal accomplishment or efficacy when our efforts are appreciated or acknowledged.
I’ve noticed that communications from employers recognize other groups of healthcare team members like nurses or medical assistants frequently and leave off physicians.
In fact, on National Physician’s Day, the communication my organization sent out thanked all members of the care team and not physicians specifically. This is not reciprocated; during medical assistant and nurses’ weeks, physicians aren’t mentioned.
One doctor on a group coaching call I was a part of was asked to sign a card on National Physician’s Day in recognition of other team members. He was quite flabbergasted.
It is an interesting dynamic that doesn’t go unnoticed. Even the one day for recognizing physicians is undermined by organizations. I’m not going to speculate here as to the reasons for these types of occurrences, but it’s important to note the trend of this sort of odd micro-aggression.
This certainly does not help physicians feel rewarded by their employers for the work they do and can lead to cynicism.
4. Community
The authors reference resources as things that enhance energy while demands (like workload) deplete energy. Social supports and community are resources that can counter depletion from demands.
They refer to community as a buffer to work demands. Community includes social support from supervisors, colleagues, other team members, and family.
The article states “a lively, attentive, responsive community is incompatible with burnout.”
How supportive is your workplace community from the administration on down to your colleagues?
Physicians are notorious for being islands onto ourselves. This is in part because we have a lot of work to do and limited time to get it done. But it’s also in part because of imposterism, which I’ve mentioned elsewhere, and perfectionism.
These two phenomena often go hand in hand but prevent many of us from discussing issues openly about our struggles or how we’re doing.
We may feel like we’re the odd duck out if we’re struggling with charts or falling behind at work. We don’t want to be perceived as weak or deficient despite telling ourselves these narratives (there is great power in narratives we tell ourselves). This keeps us from seeking help.
If I had to pick the most impactful benefit from group coaching (where individuals get coached by a coach in a setting with peers) it’s the realization of our commonality. Even within my own program, clients see that their experiences are not unique to them; many other clients will chime in that the coachee’s situation applies to them too. So many “aha” moments in these shared experiences.
Building camaraderie requires vulnerability, and that’s not something most physicians come by easily. We had to be tough and compartmentalize to get through training.
How can you help foster a better sense of community around you? It may require vulnerability on your part.
5. Fairness
Fairness is challenging to study but focuses on how leadership is perceived by physicians. It is premised on mutual trust—that consideration is given for varying needs and resources allocated in manners that don’t privilege certain groups or individuals over others.
In fact, the (negative) impact of major organizational changes can be minimized if physicians believe their leadership is fair and supportive.
This can make all the difference during a new EHR rollout and implementation or in a shift in reimbursement to more value-based contracts.
Unfortunately, other players (pharma, insurance companies and payers, PBMs, “integrators,” etc.) that have so intertwined themselves into the current healthcare system have no obligations to and thus do not give consideration to physicians and their care teams when making sweeping changes (that often increase our workloads).
Another area where mutual trust is often eroded is in physician employment and partnership contracts. Vague terms that favor employers, non-competes, prevention or limitation on outside activities, and “golden handcuffs” are but a few of the many ways physicians feel exploited when starting new jobs or renegotiating at their current jobs.
Think of the physician gender pay gap where women physicians are paid less for the same work. Or perhaps how their career opportunities are limited when they have to balance child rearing and household obligations, which disproportionately fall on their shoulders.
How is that supposed to kindle goodwill between physicians and their organizations?
6. Values
Do your values align with those of your organization?
You entered medicine in service of others’ health needs. This is what’s important to you. Are you able to feel like you contribute meaningfully in this regard?
When values match, physicians feel more connected to their organization and their work. They find meaning and purpose in healing patients. Heck, they derive joy.
I couldn’t find a GIF of stars aligning so I had to settle for planets. Although now I’m realizing usually bad things happen in movies when planets align….
On the other hand, “the smaller the overlap between individual and organizational values, the more often staff members find themselves making a trade-off between work they want to do and work they have to do [emphasis mine].”
We want to see and help patients. But seeing the patient and coming up with a care plan is such a small percentage of how we end up spending our time. We spend too much of it charting. Remember earlier when I mentioned not being able to work at the top of our licenses even most of the time?
(I suspect we name charting as the leading cause of burnout because it’s perhaps the most flagrant example of so many underlying work life area mismatches).
Another example is having to navigate around those other players in healthcare, namely insurance companies. We are often limited in our abilities to do the right thing, prescribe the right medication, etc., because of artificial barriers erected by these intermediaries.
Over time this creates value mismatch leading to disengagement and burnout. This is moral injury.
Values mismatch is what often drives physicians to leave a current job for another, or worse yet, medicine altogether.
An organization that focuses on maximizing physician time with patients and offers adequate support for handling the other bureaucratic tasks will engender value congruence and keep physicians sticking around longer (not to mention provide better care for the communities they serve).
The Silver Lining...
The first step to any problem is to define/identify it. The next step is to then uncover the underlying causes.
The good news is that Maslach and her peers have done these steps for us already.
That means we can roll up our sleeves and work on addressing them. These six areas offer entry points for change to create better workplaces to support physicians, help them thrive, and make medicine sustainable.
Improving physicians’ lot will enable us to better serve our patients. It’s not a zero-sum game; it’s a win-win.
Next week’s post will have a tool for you to use to gauge how you’re faring in these six work life areas.
So, there you have it: the six root causes of burnout. Which ones impact you the most? Let me know in the comments below!
If you haven’t subscribed to my email list, then do so below so you don’t miss my new posts or my weekly updates (only for subscribers).
I’d also be most appreciative if you shared this post with anyone whom you think would benefit from the content or message of the blog. They may similarly be most appreciative 
