This is my second post on Medscape’s Physician Burnout & Depression Report 2022 released earlier this year. The report’s tagline is “Stress, Anxiety, and Anger.”
Last week, I looked at the burnout data and offered my “hot take” that you can find here.
This week, I look at the second half of the report which focuses on depression amongst physicians. This post will be shorter than last week’s.
Note: this post will lack my characteristic GIFs due to the inclusion of images of slides from the report. That’s two weeks in a row—my cruelty knows no bounds!
Let’s get to it.
Click here to access the Medscape Physician Burnout & Depression Report 2022.
If you’re looking for the methodology and demographics of this survey (as well as general survey mocking), then head on over and read the beginning of last week’s post to find such information.
Mellon Collie and the Infinite Sadness
…is not only the title of the amazing double album that introduced me 27 years ago to my favorite band, The Smashing Pumpkins, but may also describe mental illness (depression, specifically) in physicians.
Burnout and depression are not the same, and each can exist without the other. However, they “can be causally related in both directions” [taken from the report].
Depression is a clinical diagnosis codified in the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (dubbed DSM-5). It was only recently that burnout was recognized as a diagnosis by the World Health Organization. But burnout has not yet made its way into any edition of the DSM. I am eagerly awaiting the DSM-6…said no one ever.
Turn that Upside Down into a Frown
Over one fifth (21%) of the 13,000+ surveyed physicians reported depression. Of those ~2800 physicians, about 25% reported clinical depression while almost two-thirds said they had “colloquial” depression (which I take to mean not formally diagnosed).

I wonder if it’s harder for those who diagnose depression themselves to feel like they can impartially fill out screening questionnaires and such. I’m not advocating for self-diagnosing, since it’s incredibly difficult to be objective about oneself; I’m just curious and suspect it is so.
It was Sir William Osler who said, “A physician who treats himself has a fool for a patient.”
I can’t tell for certain from the slides or accompanying commentary if this means depression at any point in their lives versus currently depressed. However, my context clue inference suggests the latter—the numbers here are physicians who are currently depressed.
How Do We Stack Up?
Other data sources suggest the lifetime prevalence of self-reported physician depression is 13% for men and 20% for women. However, this is a lifetime prevalence and not a “snapshot prevalence” like this survey.
The same reference above states that those lifetime prevalences are similar for the general population.
A better comparator for this survey is the C.D.C.’s latest survey results from 2019 in which 18.5% of US adults had “symptoms of depression,” which is slightly lower than the 21% of physicians here.
The National Institute of Mental Health estimates that 8.4% of the adult US population had major depressive disorder (MDD) in 2020.
I tried searching for estimates of MDD in physicians, and honestly, they were all over the place—some even as high as 60%!
My conclusion: the data are not robust enough on this topic.
(Ding, ding, ding! Thank you, Captain Obvious!)
Depression, in Our Words
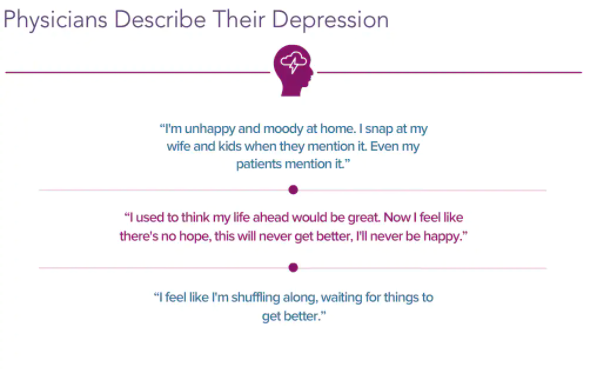
This slide stands on its own. Perhaps you’ve thought or said similar words? Perhaps you know another physician who has?
A Priori Depression?
Medscape asked respondents (presumably the 21% who previously responded in the affirmative for having depression) if they were ever depressed before becoming a physician.

Almost 40% of depressed physicians report depression even before they became physicians.
That leaves over 60% whose depression debuted since becoming physicians.
By my back of the napkin calculations, that means about 13% of all respondents experienced depression after attaining physicianhood.
Obviously, this is simply a correlation and does not imply causality—that is, that becoming or practicing as a physician caused their depression.
The Effect of Your Affect
Last week’s post mentioned the slide that briefly looked at how burnout impacted relationships.
The depression segment of the survey asked if clinical practice, specifically patient relationships, was impacted by depression.

Having depression does not mean that one cannot work effectively. That being said, I wonder what percentage cannot tell that their depression is impacting their patient interactions? Sometimes it’s hard to see something that you’re living and experiencing day in and day out without an outside perspective weighing in.
Overall, about half of depressed physicians say that their depression impacts their care along a spectrum from becoming easily exasperated all the way to making errors they otherwise would not make. And that’s a whopping 11% that think that they are making errors!
Clearly, helping physicians address mental health needs is good not only for physicians but also their patients!
Are You Assigning Yourself Wellness Modules to Complete?
Isn’t that the way to keep up your happiness and mental health?
No?
Oh, there are other ways? Are you sure? I’m skeptical, but let’s take a look:

Wait, wellness modules didn’t even make the list!
Turns out assigning additional obligations and using up more physician time does not make their lives better! This is groundbreaking!
Is that too much sarcasm? I’m sorry, sometimes I can’t help myself.
The simple tried and true—family, hobbies, exercise, sleep, and nourishment—are the primary levers physicians pull to maintain their mental wellness. This isn’t rocket science.
The commonality shared between all of these is having the time to partake in all of them.
If you spend too much of your time at work and then all of your time outside of work is still spent charting, for example, then you’re not going to have time to enjoy these restorative activities. This is a main reason I help physicians tackle their work day and get their work done at work!
What About Outside Help?
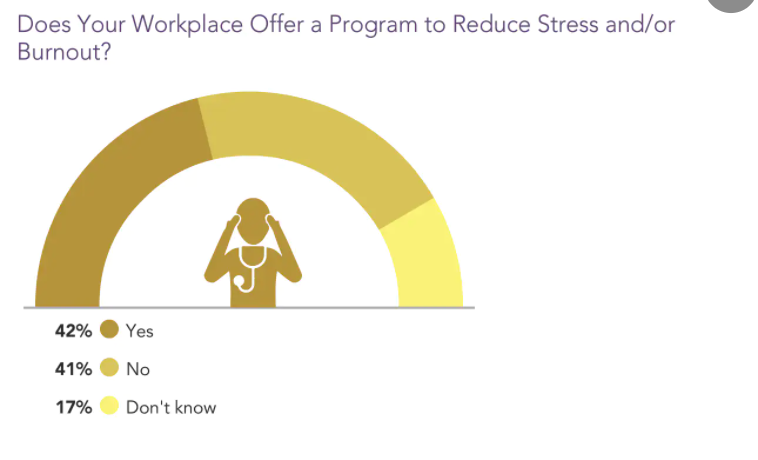
Just over 40% of physicians’ workplaces offer wellness programs that the physicians know about. A similar percentage have no such offerings from their workplace.
And 17% don’t know. Even a solid, well-designed program is of little utility if no one knows about it.
I have been generally unimpressed with most such workplace offerings I’ve seen anyway, so it doesn’t really matter whether they have one or if physicians know about them.
It often feels like organizations tout such programs to check a box that they’re doing something about burnout even if ineffectual and even as they perpetuate the culture and settings that drive burnout and moral injury in the first place.
Their time, effort, and money would be better spent addressing those issues.
This would be more than apparent if they spent time speaking with and listening to physicians. They could truly show their investment in their doctors by endeavoring sincerely to build and promote workplaces and cultures that support physician wellness.
I Fly Solo
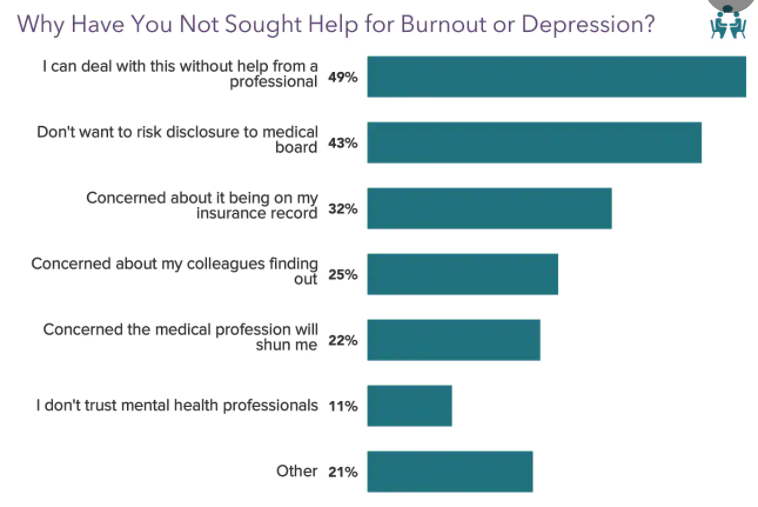
This slide is a straight up indictment of medical culture.
Half of physicians believe they can handle their mental health struggles by themselves, likely speaking to fears of appearing weak or like an imposter (do I belong if I have “made it” and feel this way?) as well as feeling shamed.
They are afraid of what their colleagues would think. They likely view it as an individual deficiency, like something is wrong with them.
Strides have been made with regards to the stigma around mental health including in the world of medicine, but those inroads are nascent and have a long way to go. Stigma is still a huge problem.
It doesn’t help that over 40% worry that many medical boards require disclosures of mental health diagnoses calling into question the capabilities of those physicians as well as negatively incentivizing to avoid labels and avoid getting help.
Per the commentary with this slide, “some physicians have reported serious career problems when mental health issues were revealed” to medical boards. It is truly perverse.
I’m not sure about the 11% that don’t trust mental health professionals!? Maybe the old guard some of whom think mental health is all quackery?
An Interesting Omission
A quick aside: this year’s report does not delve into suicide at all. Prior years’ reports actually were titled “Burnout and Suicide” reports instead of this year’s “Burnout and Depression.” I’m not sure why the change, but I thought it fascinating to point out.
I do think discussing physician suicide openly is of paramount importance given physicians die by suicide at a disproportionate and alarming rate compared to almost all other professions.
“Action is the Antidote to Despair”
While I acknowledge that me quoting this Joan Baez lyric may seem like I’m oversimplifying mental illness and reducing it to a single thing, I want to instead focus on the action part.
Because that is what I’m going to call on all of you to do—take action.
Only by advocating and pushing for change can we begin to dismantle the culture and systems that foster burnout and depression. In doing so, we can build better systems that allow us to care compassionately not only for our patients but also ourselves.
I coach a lot on wellness and advocating for ourselves in Charting Conquered because physicians deserve better. When we take care of ourselves and reclaim our time, we’re better able to care for our patients. Join the waitlist here.
And if you’re looking to learn about other ways physicians can take back control to practice medicine on their own terms, then be sure to check out the Physician Freedom Summit on March 4th and 5th.
The summit is completely free and showcases 15+ expert speakers covering topics from burnout interventions, financial independence, and physician entrepreneurship. I’ll be speaking on charting and combating burnout by reclaiming your time. Sign up here to watch the summit for free.
Physician depression is no joke; it’s effects are pervasive and far-reaching, as are its implications. I hope this post ignites a spark in you to start championing for your most prosperous life today, which includes the large chunk of time you spend at work!
I’d love to hear your thoughts on the survey or depression in general. Let me know in the comments section below.
I’d love to hear your thoughts on the survey or burnout in general. Let me know in the comments section below.
If you haven’t subscribed to my email list, then do so below so you don’t miss my new posts or my weekly updates (only for subscribers).
I’d also be most appreciative if you shared this post with anyone whom you think would benefit from the content or message of the blog. They may similarly be most appreciative 
