Hot (okay, warm) off the press, Medscape released their annual Physician Burnout & Depression Report 2022 on January 21st, 2022, with the tagline “Stress, Anxiety, and Anger.”
The report itself is presented as slides with some commentary beneath each slide. This is much akin to a Buzzfeed “top 10” list you have to click through, because nothing screams “veritable data” like Buzzfeed 
I did a post just like this last year for the 2021 report. You can find that here.
Note: this post will lack my characteristic GIFs due to the excessive number of images of slides from the report. I understand if this leaves a temporary gaping hole in your soul.
So let’s take a look at what our colleagues (including perhaps you!?) said…
Survey Says!
Yes, this report relies on the same data gathering strategy as everyone’s favorite television game show Family Feud!
Thankfully, surveys represent the créme de la créme of data generation in medicine and science, as evidenced by the quality of evidence pyramid I presented yesteryear:
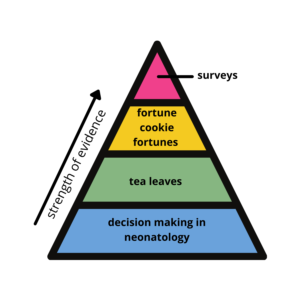
Bringing back this oldie (but goodie)
Now that we’ve established the hierarchy of evidence and I’ve reminded all neonatologists why they stopped reading this blog a year ago, let’s get to the survey! P.S. I still have nothing against neonatologists—y’all do amazing work caring for the teeny tinies!
Table 1 Deconstructed
Sarcasm aside, surveys can provide useful information despite their limitations. Let’s get some background on this survey in terms of methodology and demographics.
Medscape surveyed over 13,000 physicians (Medscape members only) representing 29 specialties via a 10-minute online survey from June 29th through September 26th, 2021.

Respondents were weighted to the AMA’s physician distribution by specialty and state to try to capture a representative snapshot of the physician community. I couldn’t find any data about how many or what percentage of US physicians are Medscape members (apparently, they’re a global company).
Sixty-one percent of respondents were male; 38% were female. I am unsure whether the remaining one percent chose not to respond or selected a non-binary response, but they didn’t make the slide.
Respondents spanned the age ranges but generally skewed older:
- <35: 5%
- 35-44: 19%
- 45-54: 25%
- 55-64: 31%
- >64: 20%
I Like My Docs Crispy
Forty-seven percent of physicians surveyed report feeling burned out, which is up from 42% last year. This is the highest overall percentage of burnout this survey has uncovered. The prior record-holder was 2015 at 46%, for reasons that are unclear to me.
Turns out a global pandemic that laid bare a multitude of failings of our healthcare system and almost crippled it entirely has taken a toll on physicians! Who’da thunk?
Other studies cite burnout rates up to 80%, so I don’t know if the Medscape respondents are the Pollyannas of the bunch or what?
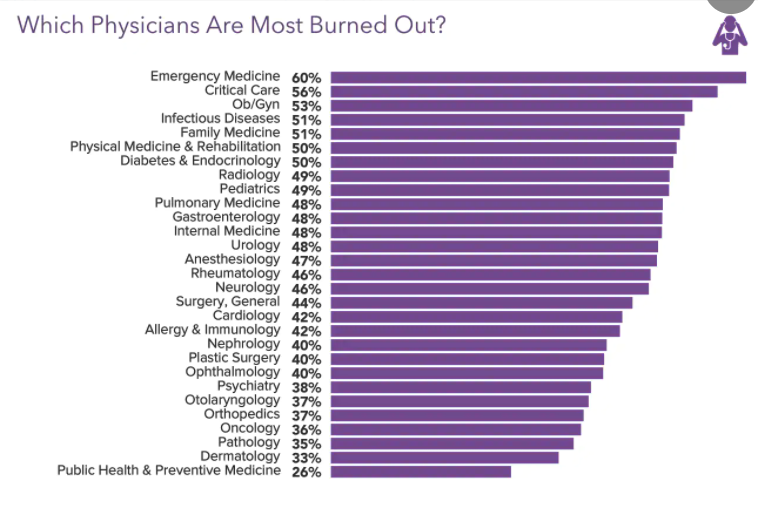
This year Critical Care docs dropped to second as Emergency Medicine physicians skyrocketed to claim the number one spot. No surprise there.
Honestly, so many different specialties could be in the number one spot.
Primary Care specialties remain all near the top as well.
Bringing up the rear are Dermatology and Public Health/Preventive Medicine—not sure how the latter aren’t burning out during a public health emergency?!
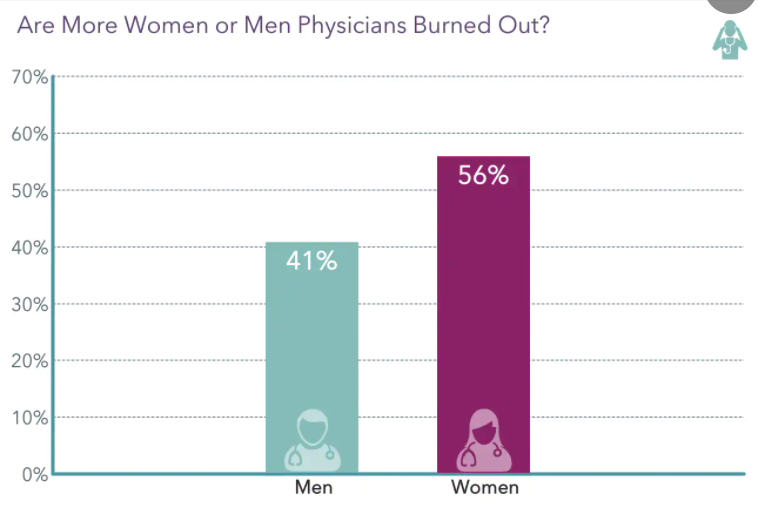
Rates of burnout increased by 5% for both women and men physicians, now up to 41% of men and 56% of women. The burnout gap between men and women persists.
The reasons for this are myriad—including the gender pay gap, societal expectations including taking care of the household, maternity leaves, etc.—on top of which COVID stressors kept children at home (necessitating childcare and distance learning), which likely overwhelmingly fell on the shoulders of women physicians compared to men physicians.
A Kaleidoscope of Mope
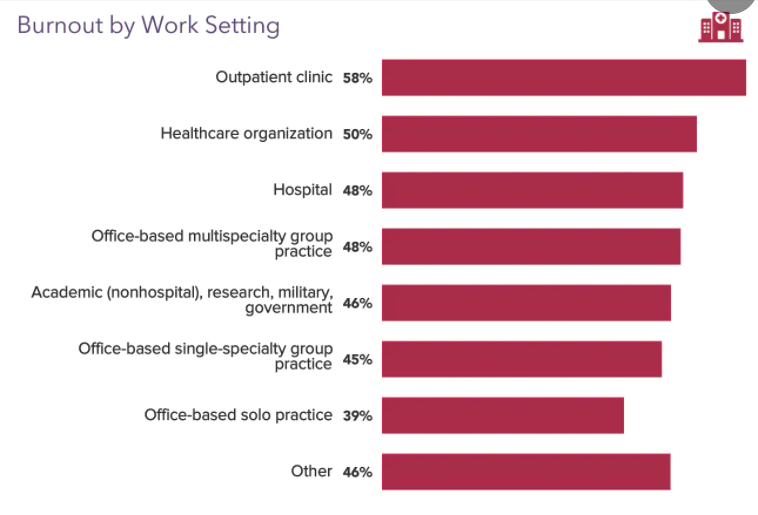
It’s selfishly validating that outpatient clinics take the cake for the biggest burnout factories at 58%, up from 46% a year prior!
Anecdotally, I found that patients always understood that local area hospitals were overrun and understaffed but rarely extrapolated that to what must be going on in the clinics.
And that’s no fault of their own—news coverage was almost entirely about hospital-based care.
But it’s not a competition; most settings didn’t do well and contributed to their physicians burning out.
I’d like to point out that some of these responses are not mutually exclusive. For example, working in a “healthcare organization” could mean working in a clinic or hospital capacity, no?
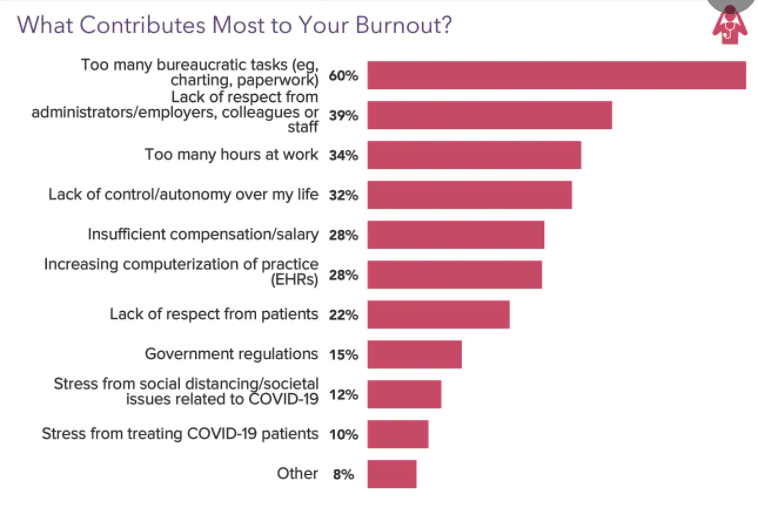
The leading cause of burnout remains “too many bureaucratic tasks.” This includes charting, rifling through paperwork to find the damned signature lines, submitting prior authorizations for medications our patients need, trying to cram in peer to peer calls, and checking or clicking endless boxes to satisfy some metric or another.
Historically, the second leading contributor was spending too much time at work…because of all the bureaucratic tasks without adequate support.
However, this year “lack of respect from admin/employers, colleagues, or staff” claimed the second spot. I can only imagine that this contributor worsened primarily due to lack of respect from admin/employers, with physicians feeling the sting of pay cuts, inadequate PPE (at least earlier on), lack of much needed flexibility, being asked to do ever more with ever less, and “business as usual” attitudes (despite the world seemingly going to hell in a handbasket several times over).
We Don’t Talk about Burnout, No, No, No
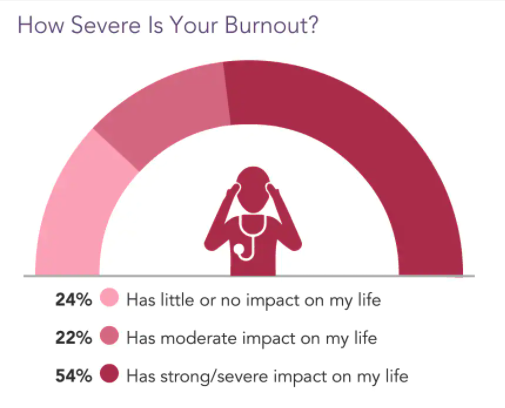
Over half of the respondents reported that their burnout had a strong or severe impact on their lives. Over three-quarters of physicians reported at least a moderate impact on their lives.
Burnout is pervasive not only in its ubiquitousness amongst physicians but also with the breadth in how it affects those physicians.
This is made clear by the next graphic: burnout not only impacts the physicians, but also those around them.
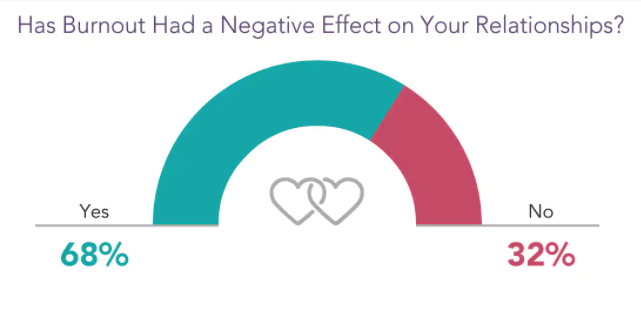
For those physicians suffering burnout, over two-thirds reported that it negatively impacted their personal relationships. It is clear that we bring our work home in more ways than one, and in more detrimental ways than just having to stay up writing notes.
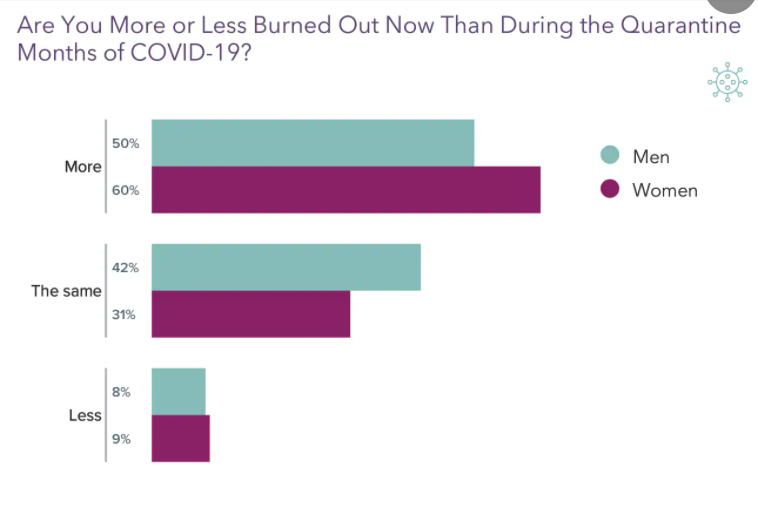
Medscape differentiates between the “quarantine” period of the pandemic (mostly 2020) and the “back to work” period (i.e., 2021).
More physicians reported burnout last year during the “back to work” period while navigating the constant restructuring and adjusting demanded by the mercurial COVID-19 pandemic.
The numbers are quite impressive: 50% of men and 60% of women physicians reported more burnout in 2021 compared to 2020.
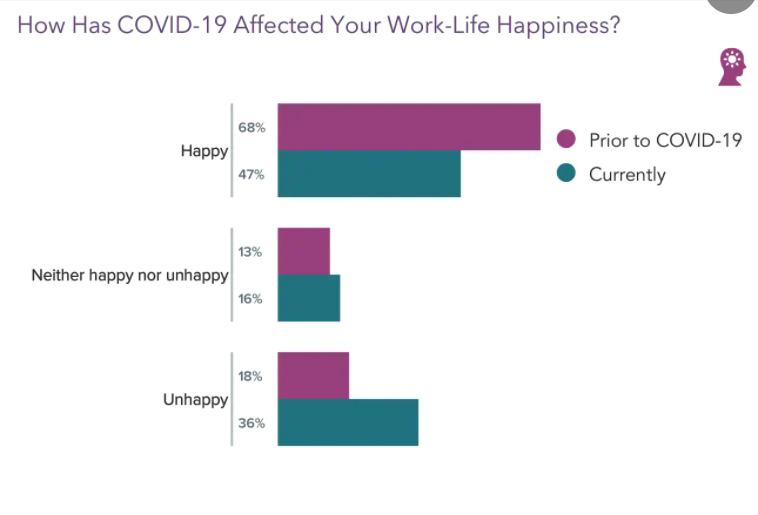
The physicians surveyed shared that their work-life happiness dropped because of the pandemic. Again, this is not revelatory.
Two-thirds reported being happy pre-COVID. That number dropped to less than half as the pandemic continues.
Importantly, twice the number of physicians reported being unhappy now compared to pre-COVID, up from 18% to 36%!
You Gotta Fight For Your Right…To Avoid Burnout

It is encouraging to see that not all physicians sit idly by in their suffering. A good number take action at work to remedy their situations. However, over one-quarter do nothing to change their lot.
Directly reducing exposure to the noxious stimuli by reducing work hours remains the most common action taken (though now tied with stress reduction techniques), and given the lack of headway usually seen with the other forms of action to alleviate burnout, this is hardly shocking.
Unfortunately, the reduction in work hours does not result in a proportional reduction in work. This was not part of the survey but simply my observations of others I coach and my own experience in the clinic setting.
When outpatient doctors cut back our hours, we have the same number of patients, refills, and forms to see, fill, and complete—we just now have less time to do it.
Meditation and stress-reduction techniques are effective tools, which is why we’ve seen an uptick in their utilization.

While the prior graphic focused on work-based burnout busters, this one instead looks at what physicians do on their own time to cope with burnout.
As you see, this list includes healthy as well as unhealthy coping mechanisms.
The healthy ones include exercising, talking with confidants, sleeping, and music (hey, I do that!).
The unhealthy ones include isolation and buffering or numbing with substances.
Wait, If You Ask What People Need…They’ll Tell You?!
Mind blown!
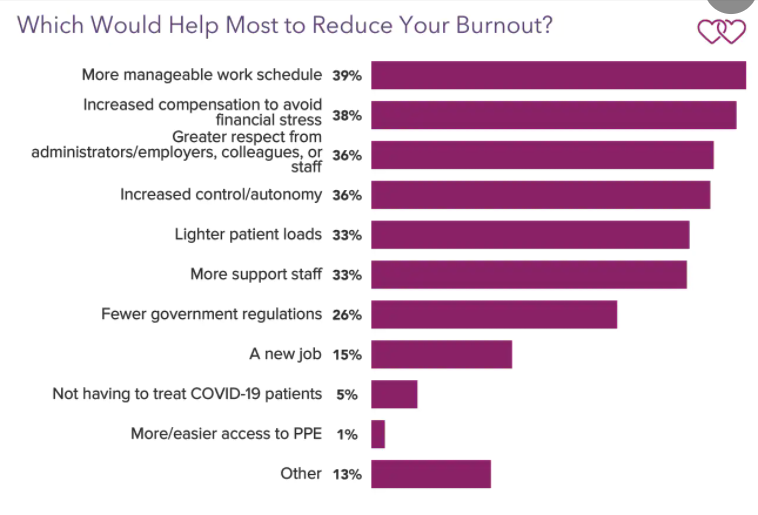
Last year, the leading response to this question was increased compensation, so I’m glad to see that a “more manageable work schedule” has topped the list this year.
In last year’s post, I explained why I thought physicians missed the mark thinking increased compensation is the most important thing:
[Physicians] think increased compensation will make them like their jobs more even though it won’t address the root causes of their burnout.
Don’t get me wrong—higher compensation would be awesome and if saved appropriately can put physicians on more secure footing to negotiate from a place of power. But getting paid more won’t make them resent the job less or alleviate the misery.
Thankfully, the rest of the responses would actually reduce burnout and make a career in medicine more sustainable.
Notice how none of the responses include building resiliency, work-mandated wellness modules, or being lectured into doing yoga?
Hint: if you lead physicians in any capacity and are serious about addressing burnout, then look at this list carefully.
Out of Nowhere!
I made a compelling argument in last year’s post on the role of coaching (seriously, go check it out), and lo and behold—coaching made the survey this year!
Maybe Medscape read my post from last year!? Nahhh.
But this is a very exciting development that is becoming more mainstream.

Eleven percent of respondents said they had used a service (including possibly a coach) to help reduce burnout!
More importantly, 46% said they would consider using such services!
Now I obviously have a huge conflict of interest here, but the only reason that conflict exists is because I believe that coaching is such a powerful weapon in our arsenal to combat burnout, especially when the coaching is done by a physician.
C-suite execs, including those in healthcare companies, have executive coaches; it’s almost become an expectation that C-suiters are provided coaching.
So why not the actual leaders of healthcare?
I would have loved a few follow-up questions for those who partook in such services:
- What was your result/did it help?
- Would you recommend it to other physicians?
“The Wind of Change”
This rock ballad by the band Scorpions captured the ethos of the end of an era of darkness and the emergence of hope. For this German band, the former meant the end of the Cold War and the latter the reunification of Germany.
(The irony/sadness of the timing of this reference is not lost on me as Russia currently seeks to restore a Soviet-esque hegemony with its invasion of Ukraine.)
Reflecting on the report’s tagline—stress, anxiety, and anger—I can’t help but feel that change is afoot. And not in spite of those feelings, but more so because of those feelings (especially anger).
Elsewhere I’ve made the case that we cannot sit back and wait for “benevolent” players to make the system better for us, thinking that they have to take action because the system is simply untenable.
It’s not in the interest of many of those players—hell, half of them profit off of the dysfunction of our healthcare system; it’d be like sawing off their money making leg for them to advocate for change.
Instead, it’s up to physicians to push back to once again make physicians and patients the center of healthcare. A large part of that endeavor has to acknowledge our own humanity and prioritize the other aspects of our lives—we are not solely defined by being physicians.
I see inroads being made via physician entrepreneurship, of which I am but a small part. Entrepreneurship is simply a vehicle for detethering us from our day jobs, but it’s not for everyone.
Other physicians are detethering themselves via diversified streams of income including real estate investing and other means. This helps them operate from a more empowered space, and many are using that space to advocate for their fellow physicians.
Yes, change is afoot. But we must all work together to create the overhaul we want to see. And it starts with advocating for ourselves at work. Let’s put that stress, anxiety, and anger to good use.
I coach a lot on this subject in Charting Conquered because physicians deserve better. When we take care of ourselves and reclaim our time, we’re better able to care for our patients. Join the waitlist here.
And if you’re looking to learn about other ways physicians can take back control to practice medicine on their own terms, then be sure to check out the Physician Freedom Summit on March 4th and 5th.
The summit is completely free and showcases 15+ expert speakers covering topics from burnout interventions, financial independence, and physician entrepreneurship. I’ll be speaking on charting and combating burnout by reclaiming your time. Sign up here to watch the summit for free.
I hope this post examining Medscape’s most recent survey on physician burnout was enlightening. While I try to infuse some humor and levity into my writing, know that this issue is near and dear to me and that I find this work to be of the utmost significance.
I’d love to hear your thoughts on the survey or burnout in general. Let me know in the comments section below.
If you haven’t subscribed to my email list, then do so below so you don’t miss my new posts or my weekly updates (only for subscribers).
I’d also be most appreciative if you shared this post with anyone whom you think would benefit from the content or message of the blog. They may similarly be most appreciative 
