Hot off the press, Medscape released their annual National Physician Burnout & Suicide Report 2021 on January 22nd, 2021, with the tagline (not sure what it’s called when it precedes the main report name?) “Death by 1000 Cuts.”
That cheery tagline came from a physician’s comment in the survey, which implied that everything about the physician work day contributes to burnout.
This post will examine the first half of the report only, which focuses on burnout. I will leave alone the depression and suicide material for now.
The report itself is presented as slides (like a Buzzfeed “top 10” list you have to click through) with some commentary beneath each slide.
Please note: I don’t want to dive into the appropriateness of the nomenclature, suffice it to say I think it’s fine to call it “burnout.” I do agree that the term “moral injury” better encapsulates the true pervasive nature and extent of the effects of burnout. However, “burnout” will be used for this post since it is used in the report we will explore.
Also note: this post will lack my characteristic GIFs due to the excessive number of images of slides from the report. I understand if this leaves a gaping hole in your soul. Just remember, it’s only for this week and the GIFs will return next week!
Final note: all images (except the blog title image and the first image that I created) come from the linked Medscape report.
So let’s take a look at what our colleagues (including perhaps you!?) said…
Click here to access ‘Death by 1000 Cuts’: Medscape National Physician Burnout & Suicide Report 2021
Please note that the link above is to a Google search for the article as linking directly to it requires a Medscape login. It is currently the first hit.
Let's Hear It for Surveys!
As we all know, surveys are the paragon of quality we rely on to advance medicine and science. They sit atop the pyramid in terms of quality of evidence.
Oh, they don’t? Are you sure? I’m not sure what pyramid you’re using, but surveys are certainly at the top of mine.
I made this on my phone…seriously!
Now that we’ve established the hierarchy of evidence and I’ve earned the scorn of all neonatologists, let’s get to the survey! P.S. I have nothing against neonatologists—y’all do amazing work caring for the teeny tinies!
Table 1, But Not in Table Form...
Sarcasm aside, surveys can provide useful information despite their limitations. Let’s get some background on this survey in terms of methodology and demographics.
Medscape surveyed over 12,300 physicians (Medscape members only) representing 29+ (not sure why 29+ and not, I dunno, 30?) specialties via a 10-minute online survey from August 30th through November 5th, 2020.
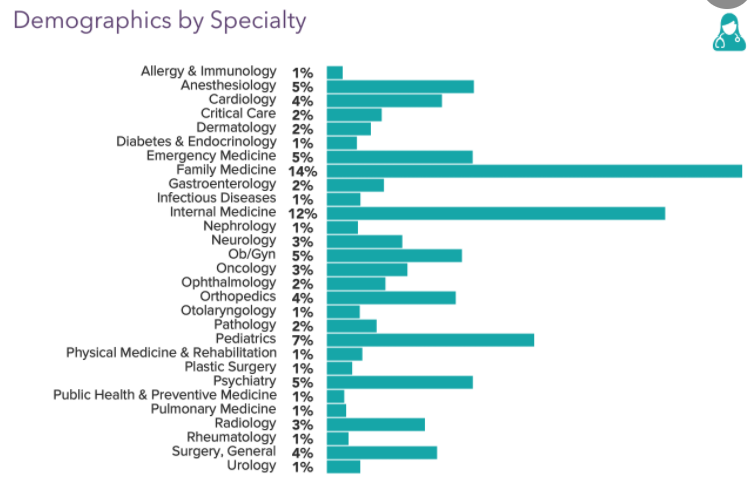
Respondents were weighted to the AMA’s physician distribution by specialty and state to try to capture a representative snapshot of the physician community. I couldn’t find any data about how many or what percentage of US physicians are Medscape members (apparently, they’re a global company).
Sixty-one percent of respondents were male; 37% were female. I am unsure whether the remaining two percent chose not to respond or selected a non-binary response, but they didn’t make the slide.
Using Medscape’s definitions of generations from their 2020 report, the 2021 breakdown of respondents was as follows: 17% were millennials (25-39yo), 36% Gen Xers (40-54yo), and 47% Boomers (55-73yo).
Burnin' For You
Forty-two percent of physicians surveyed overall report feeling burned out, which is the same as in 2020. I find this shocking since the 2020 data collection period was in 2019, i.e. pre-COVID.
This percentage is down from 44% in 2019 and 46% in 2015, which again baffles me. There was no commentary examining why the percentage is dropping even during a global pandemic that has shaken our healthcare system to its core and taken a severe toll on physicians.
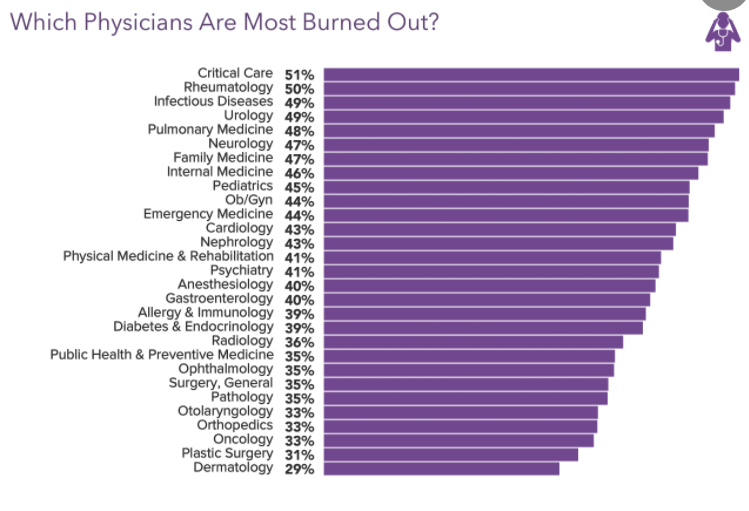
Not surprisingly, Critical Care docs moved to the top of the list this year with the pandemic, ousting the former crispiest docs, the Urologists.
Primary Care specialties are all near the top as well.
Bringing up the rear are the “most superficial” (get it?) physicians, the Plastic Surgeons and Dermatologists!
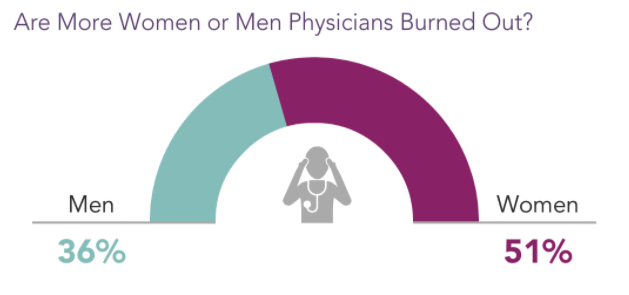
Over half of women physicians report feeling burned out compared to just over one-third of men physicians. Compared to years prior, more women physicians are reporting burnout, so the gap between men and women is widening.
The reasons for this are myriad—including the gender pay gap, societal expectations for taking care of the household, maternity leaves, etc.—on top of which COVID stressors kept children at home (necessitating childcare and distance learning), which likely overwhelmingly fell on the shoulders of women physicians compared to men physicians.
Why the Long Face?
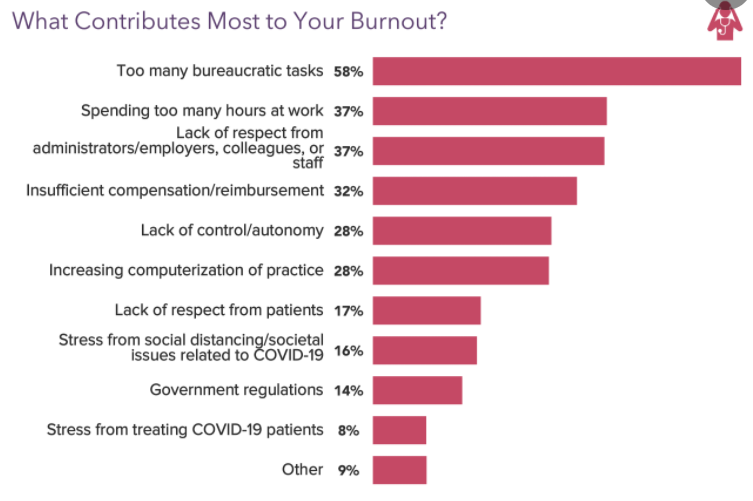
The leading cause of burnout is “too many bureaucratic tasks.” This includes charting, rifling through paperwork to find the damned signature lines, submitting prior authorizations for medications our patients need, and checking or clicking endless boxes to satisfy one metric or another.
The second leading cause ties in directly with the first—spending too much time at work…because all the bureaucratic tasks waste so much time without adequate support.
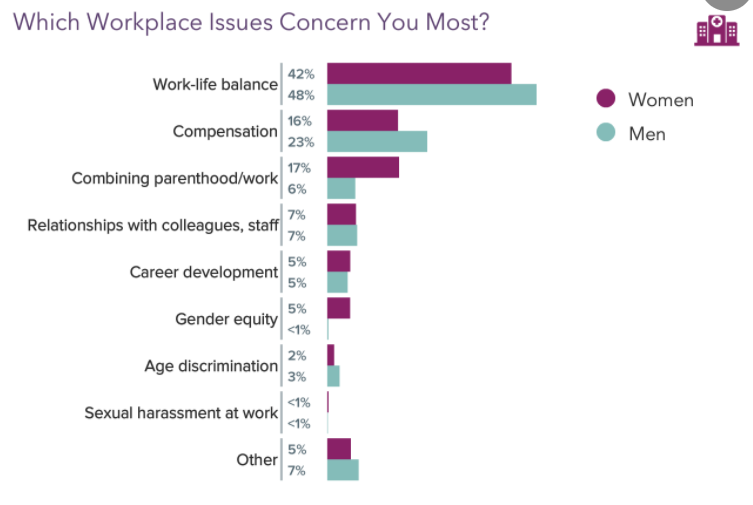
The issue most important to physicians is the ever-elusive “Work-life balance” (at some point in the future I’ll share my thoughts on why I find this term/idea misleading).
Interestingly, men physicians reported this more than women physicians, which may seem confusing given what we’ve discussed above about women physicians.
However, the report separates out “Combining parenthood/work” (shouldn’t this be included in work-life balance?), which was reported as the biggest issue to three times as many women as men.
If combined with “Work-life balance,” then it would be the leading issue for 59% of women compared to 54% of men.
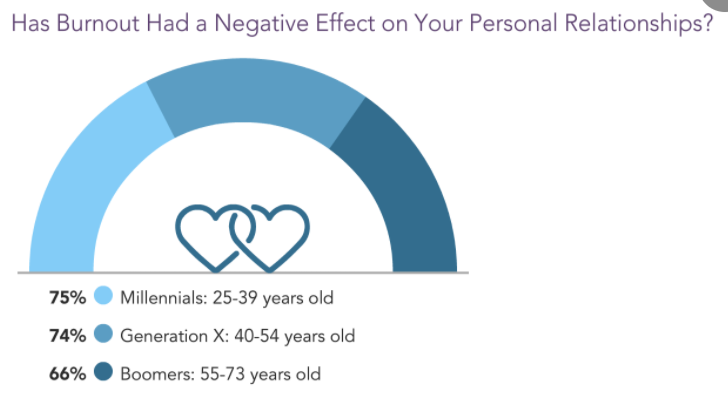
For those physicians suffering burnout, two-thirds to three-quarters (based on generation) reported that it negatively impacted their personal relationships. It is clear that we bring our work home in more ways than one, and in more detrimental ways than just having to stay up writing notes.
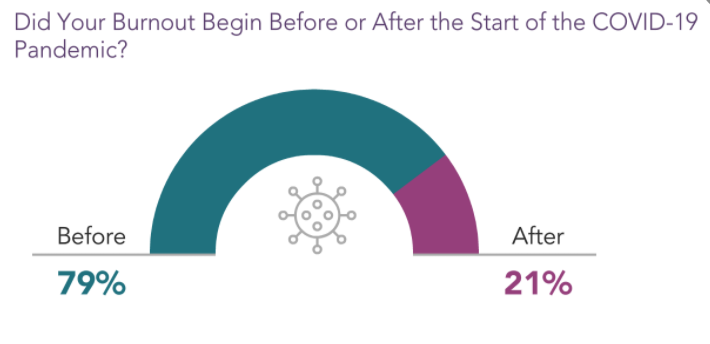
More physicians reported burnout last year after the COVID-19 pandemic upended not only our home lives but also our work lives. Not sure how this relates to the fact that fewer physicians are reporting burnout overall? This definitely does not square away with that.
We're Not Gonna Take It...Unless We Have To?

It is encouraging to see that not all physicians sit idly by in their suffering. A good number take action to remedy their situations. However, over one-third do nothing to change their lot.
Directly reducing exposure to the noxious stimuli by reducing work hours is the most common action taken, and given the lack of headway usually seen with the other forms of action to alleviate burnout, this is hardly shocking.
Unfortunately, the reduction in work hours does not result in a proportional reduction in work. This was not part of the survey but simply my observations as well as now my own anecdotal experience having cut back my hours just a few weeks ago to kick off 2021.
(The Coach in Me is the Coach in You)
Forcing a lyrical analogy to try to make a theme out of this post? Who, me?
Just a brief aside to bring in the coaching element. Changing your circumstances before you’ve done the mindset work to understand that your circumstances don’t control your feelings usually does not change anything.
By this I mean if you change jobs—which is what I assume they mean by “Changed work settings”—due to burnout without addressing your internal negative monologue that burnout generates and perpetuates, then you’ll likely find yourself in the same situation.
Only now you think it’s hopeless because even a more promising job led to the same results. Or worse yet, you think there’s something wrong with you.
So before making any job transitions, make sure you’re not relying on a classic arrival fallacy that once you change jobs everything will magically be better. Instead, examine what thoughts underlie your feelings and know that you have control over your thoughts no matter the circumstance.
Then you can make your decision from a place of strength, self-compassion, and peace.
Misguided Muse
Sadly, when queried what would help most to reduce burnout, most physicians miss the mark, in my opinion.
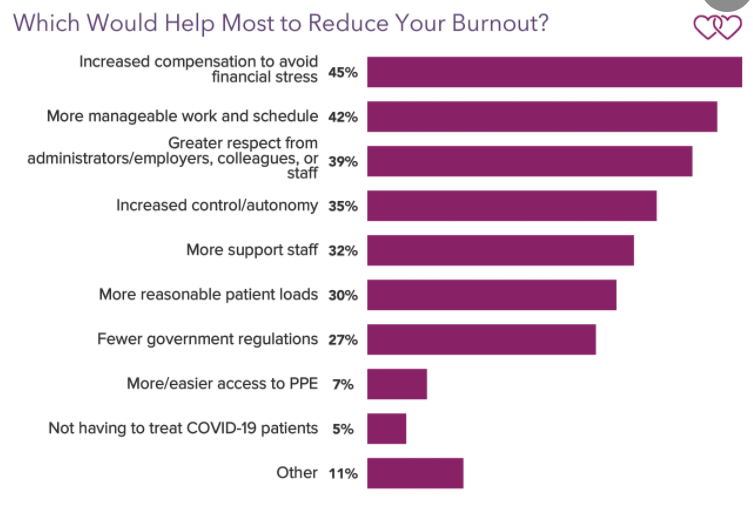
They think increased compensation will make them like their jobs more even though it won’t address the root causes of their burnout.
Don’t get me wrong—higher compensation would be awesome and if saved appropriately can put physicians on more secure footing to negotiate from a place of power. But getting paid more won’t make them resent the job less or alleviate the misery.
Thankfully, the rest of the responses starting with #2 would actually reduce burnout and make a career in medicine more sustainable.
You may question the third response about “Greater respect,” but most physicians feel like interchangeable cogs in a machine based on how they’re treated by their employers.
This drains the joy and purpose from the practice of medicine, leaving many with a very unbalanced experience of the career to which they’ve devoted so much time and effort.
The desire for greater respect also stems from a place of wanting to be afforded the autonomy to practice medicine as the art that it is, and not simply as a set of protocolized algorithms that cannot possibly best serve every patient and their unique needs.
The Times They Are A Changin'
As I wrap this post with my finals thoughts, I can’t help but go back to that tagline: Death by 1000 cuts.
Every little thing adds up. Every. Little. Thing. Hurts.
But there is hope.
Awareness around this is growing and physicians are pushing back. Losing a physician costs an institution a sizeable six- to seven-figure sum (factoring in downstream revenue from ancillary services and testing, etc., ordered).
Institutions are recognizing this more and more however reticent they are to accept that organizational structure and culture are the actual drivers of burnout, not individual “hypo-resiliency.”
Younger physicians are putting a greater emphasis on prioritizing home life as well. Physicians are speaking out and taking matters into their own hands for themselves and for their patients.
For example, the direct care (e.g., direct primary care) movement is afoot and gaining momentum as a private practice model to disintermediate insurance companies and healthcare organizations out of the physician-patient relationship.
Doctors are seeking diversified streams of income including real estate investing and side gigs (like this one!) so as not rely solely on their clinical income. I’m convinced that the more doctors that enter the entrepreneurial space, the faster we will find creative solutions to burnout.
The collective physician will eventually will lead to changes that not only protect our patients, but also our ability to care for our patients in a satisfying and humane manner. That allow us to reclaim medicine.
While we have allies, we cannot rely on others to do this work. We must ourselves endeavor for this change.
It will not be easy, but we are doctors and we know hard work.
I hope this post examining Medscape’s most recent survey on physician burnout was enlightening. While I try to infuse some humor and levity into my writing, I know this issue is of utmost significance, so please don’t confuse my attempts at entertaining for flippancy. This is near and dear to me.
I’d love to hear your thoughts on the survey or burnout in general. Let me know in the comments section below.
If you haven’t subscribed to my email list, then do so below so you don’t miss my new posts or my weekly updates (only for subscribers).
I’d also be most appreciative if you shared this post with anyone whom you think would benefit from the content or message of the blog.
